Welcome to the second edition of The Kidney Quarterly, a new publication dedicated to stories that highlight the Can-SOLVE CKD Network’s impact on Canadian kidney health research.
We are pleased to launch this issue on June 21, which is National Indigenous Peoples Day. It is a time to honour the history, heritage and diversity of Indigenous peoples. In this issue, we highlight several projects and initiatives focused on improving the kidney health of Indigenous peoples. We are committed to working with Indigenous patient partners, Knowledge Keepers, community leaders, academics, and health care providers to ensure the best kidney health outcomes, while ensuring Indigenous knowledge and perspectives are reflected across our research projects and governance.
Special message
A message from the Indigenous Peoples’ Engagement and Research Council (IPERC)

By Craig Settee,
Indigenous Peoples’ Engagement and Research Council Coordinator
Tansi, Aniin, Boozhoo, Hello. I would like to acknowledge and greet you from the traditional, unceded territory of the Coast Salish Peoples, home of the Musqueam, Tsleil-Waututh, and Squamish First Nations.
June is National Indigenous History Month which is a time to honour the history, heritage and diversity of Indigenous peoples. June 21 is National Indigenous Peoples Day and is a time for all Canadians to recognize and celebrate the unique heritage, diverse cultures and outstanding contributions of Inuit, Métis and First Nations. Ways to celebrate or commemorate Indigenous peoples can take place, not only this month, but throughout the year. I encourage you to check with your local Friendship Centre and other Indigenous community organizations for ways to support local Indigenous initiatives such as businesses and artists.
As we celebrate the achievements of Indigenous peoples, we must also acknowledge our history which includes the impact of colonialism. The uncovering of the remains of 215 Indigenous children at the Kamloops Indian Residential School is a stark reminder of the devastating impact of the residential school system. This is an issue that affects all Canadians; it is not only an Indigenous issue. It is our shared history. How might you begin to learn, or re-learn, the history of Indigenous peoples? Online training resources include OCAP (Ownership, Control, Access, Possession) and San’yas Indigenous Cultural Safety Training which provide foundational teachings on the histories of Indigenous peoples, their cultures, health and data sovereignty.
Indigenous Research Ethics and Protocols is a free three-part webinar series with Dr. Malcolm King, and aims to help research teams acquire skills to respectfully engage with Indigenous peoples. The NCTR – National Centre for Truth and Reconciliation is another online space to learn more during this National Indigenous History Month and throughout the year.

The Indigenous Peoples’ Engagement and Research Council (IPERC) and other Can-SOLVE CKD Network members at the 2019 Can-SOLVE CKD Annual Meeting
There are many steps in the path towards reconciliation. Building respectful relationships and working in collaboration with Indigenous peoples is the first step of many. I am grateful of the Indigenous initiatives throughout the Can-SOLVE CKD Network including Kidney Check, Treatment Options and iCARE. I wish to give thanks to the Indigenous patient partners and researchers throughout the network who are involved in these projects and committees working to improve quality of life and lead to better Indigenous health outcomes for kidney health research in Canada.
I give thanks to the committee members of IPERC who strive to ensure the unique needs and perspectives of Indigenous peoples are appropriately incorporated, addressed and respected. Members of the council include patients, families, caregivers, Knowledge Keepers and health professionals including nurses, doctors, and policy/decision makers.
Important work I would like to highlight is the Wabishki Bizhiko Skaanj (wah-bish-kih biish-ih-goo skaa-nch) Learning Pathway which aims to enhance researchers’ knowledge and awareness of racial biases, Indigenous voices and stories, the impact of colonization on Indigenous health, and culturally safe health research practices. There are various learning markers which encourage participants to look, listen, learn, and lead their way along the pathway.
Look within to observe and examine racial identities, privileges, and biases. Listen to Indigenous voices and stories by participating in interactive learning exercises, facilitated online modules and webinars. Learn by enhancing your knowledge of the history of colonization in Canada and its impacts on Indigenous peoples and their health. And last, but not least, lead by reflecting on the learning and making a commitment to take appropriate actions that will build genuine partnerships with Indigenous peoples and communities in the spirit of reconciliation.
Please visit wordpress-617525-2003857.cloudwaysapps.com/learning-pathway on this National Indigenous Peoples Day. I encourage you to begin, or continue your journey, along the learning pathway as a step towards reconciliation.
Miigwetch, Ekosani, Thank you.
“There are many steps in the path towards reconciliation. Building respectful relationships and working in collaboration with Indigenous peoples is the first step of many.”
Craig Settee
Indigenous Peoples' Engagement and Research Council Coordinator
Feature story
New webinar series aims to inspire a deeper understanding of land acknowledgments

Most Canadians are familiar with land acknowledgments, whereby the traditional Indigenous territories are acknowledged before meetings, conferences, or other gatherings. But what is the true purpose of these acknowledgments and what do they mean to each of us?
At the most basic level, this practice brings to light the historic and current presence and stewardship of First Nations, Inuit and Métis people over the land. But, in truth, acknowledging the land has a much deeper meaning and purpose.
“Indigenous people have been invisible and misrepresented for decades, centuries really, and so land acknowledgment is a practice of acknowledging, honouring, respecting, and reclaiming those spaces that Indigenous peoples have occupied for time immemorial, and continue to do so,” explains Catherine Turner, a Métis woman and Senior Research Coordinator of Can-SOLVE CKD’s Kidney Check program.
For non-Indigenous people, saying a land acknowledgment can be difficult. It may involve directly or indirectly reflecting on the pain and suffering that colonization has caused for generations of Indigenous people, which is a difficult truth to confront.
“Being aware of history, true history, and realizing that it was different from what we were taught growing up is very important,” explains Mary Beaucage, an Anishinaabe woman from Nipissing First Nation (Robinson-Huron Treaty Territory) Ontario, Canada, and co-chair of Can-SOLVE CKD’s Indigenous Peoples Engagement and Research Council (IPERC). “There’s a rich history here and that has to be acknowledged and has to be brought [back] to life.”
To support members of Can-SOLVE CKD in understanding the importance of land acknowledgments, a working group of Indigenous and non-Indigenous members came together to create a new, four-part webinar series. After several months of busy planning, the webinar series is set to launch this summer.
The first webinar includes a panel of Can-SOLVE CKD members (including a researcher, patient partner and member of the Operations team) and cultural safety educator Harley Eagle of the Dakota/Ojibway First Nations, enrolled in the Whitecap Dakota First Nations Reserve. Mila Tang is a Project Manager with Can-SOLVE CKD who participated on the panel. She says that while it was an honour to participate, she knew the process would also challenge her. “I came into this project knowing that I had to be vulnerable to discomfort for personal growth to happen,” she explains.
Some key themes that she highlights after working on this project include reflecting on the meaning behind “unceded territory,” the history behind the land on which she stands, and how the land was in its natural state before colonization. She also notes that this was a chance to explore her own personal ties to the land, and reflect on the ways in which it nourishes and sustains life. “Without acknowledging the importance of how land plays such a big part in our human experience, we take it for granted,” she says.
The second webinar includes teachings from two Knowledge Keepers, who discuss important topics such as traditional protocols for visiting the land of a neighbouring First Nation, as well as historical land dispossession experienced by Indigenous people. In the third webinar, Indigenous scholars dig deeper into land disposition issues, including how resource extraction affects Indigenous people. As well, they discuss the impact of treaties and the importance of water in land acknowledgments.
The final webinar is hosted by IPERC Coordinator Craig Settee, who is Cree/Anishinaabe and a registered member of Fisher River Cree Nation (Treaty 5 Territory), Manitoba, Canada. He provides a general overview of the webinar series and encourages people to take land acknowledgments one step further – by taking action on Truth and Reconciliation Commission recommendations.
“Land acknowledgments are a first step of many,” he emphasizes, noting that there are a number of Indigenous communities that are calling for actions to return land. “Part of allyship can be supporting Indigenous movements of returning land back to Indigenous people.”
To further support people in this process, the Land Acknowledgment working group is putting together a guidebook, which will summarize some key aspects of the webinars, include reflection questions, and direct people to resources for additional information and learning. All Can-SOLVE CKD members are encouraged to participate in the webinar series and explore their own thoughts and actions related to land acknowledgments.
Notably, this series was created out of a learning opportunity. Beaucage facilitated a land acknowledgment exercise with a group of non-Indigenous researchers and noticed some fumbling and awkwardness. She took the opportunity to write a letter to the group, many of whom had little exposure to acknowledging the Indigenous land they were living on. She wanted to educate people on the importance of land acknowledgements and how to do them respectfully. The letter served as a catalyst for the new webinar series and became the narration of the series’ introductory video.
“We don’t tell people that it’s prescriptive or in a certain format, because there has to be part of your heart in there as well,” explains Beaucage. “But it was more so to give people understanding and confidence in feeling that they can do this and they can do it well.”
Tang notes that land acknowledgments are an important opportunity to explore truth and awareness. She says, “If done authentically, it is an act of humility and gratitude, being curious of what we don’t know, a reminder of our dependence on the land, and inspiring others to do the same.”
“Being aware of history, true history, and realizing that it was different from what we were taught growing up is very important. There’s a rich history here and that has to be acknowledged and has to be brought back to life.”
Mary Beaucage
Co-Chair, Indigenous Peoples’ Engagement and Research Council
Co-Chair, Patient Governance Circle
Feature story
Kidney Check program explores safe ways of engaging Indigenous communities during COVID-19

In March 2020, Can-SOLVE CKD’s Kidney Check program had already screened more than 130 individuals in rural and remote Indigenous communities and was poised to be implemented on an even wider scale.
But like many projects during this time, COVID-19 disrupted plans abruptly – prompting the program’s coordinators to find new ways of partnering with First Nations communities to continue kidney screening.
One of the best ways to treat kidney disease is to identify it early and take preventative measures to slow disease progression. Yet many First Nations people, who are disproportionately affected by kidney disease, are living in remote communities and lack access to adequate kidney health screening and care. The Kidney Check program aims to address this problem by supporting First Nations communities in implementing local kidney health screening.
Catherine Turner is a Métis woman and the Senior Research Coordinator of the program in British Columbia. On March 13, 2020, she had just returned home after visiting a First Nations community that was about to implement the program. “The intention was to begin in-community screening the following week, but because of COVID we had to cancel,” she explains. “It was a new situation, nobody knew what it was going to look like in terms of the project.”
Turner’s team began exploring ways that the program could continue to be delivered safely from afar. Kidney Check screening can be done by a local nurse who is already familiar with the community and who receives training through the program, or an external nurse who is brought in. This prompted the Kidney Check team to explore which community nurses would be potentially interested in virtual training sessions and moving forward with screening. “Some of the communities were more responsive to the idea and felt that they had the capacity to carry out screening. So as a team, [we] started to look at the option of a virtual training session,” says Turner.
They went on to develop a virtual training session program, which has already been successfully implemented for one First Nations community in BC, and the team plans to host another session with a separate community in July. Turner notes that the virtual sessions are less personal and do not allow for the practice of ceremonies, which is important for creating culturally safe spaces; however, she anticipates reengaging with these important in-person aspects of the program once COVID cases are lower and it is more safe to do so.
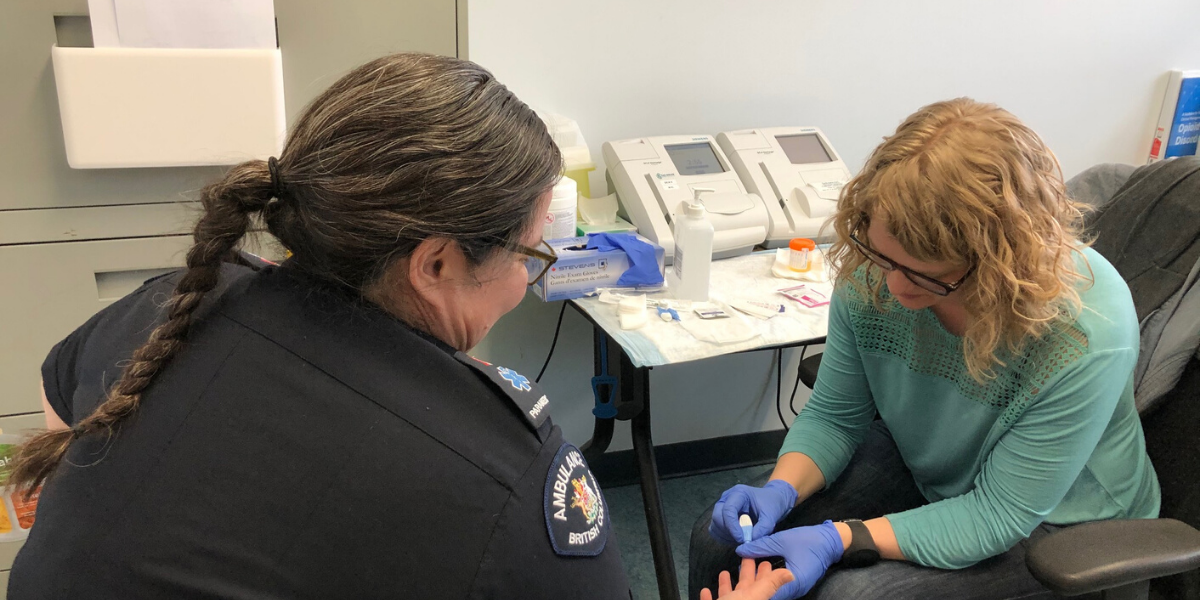
A Kidney Check screening event in 2019
Heather Martin is the coordinator for the Kidney Check program in Manitoba, which is also adapting the program during COVID-19, but in a slightly different way. “The Manitoba team will use an integrated dataset containing population-level administrative health data that will allow us to find individuals with risk factors of chronic kidney disease and connect with them by mail,” she explains. “After being contacted, the individual can determine whether they would like to participate in screening and will have their lab tests done locally to initiate their kidney health check.”
She says her team expects that this approach will discover 20,000 to 30,000 adults in Manitoba and a trial sample of just over 3,000 will have kidney health checks by either their primary care team or directly with a physician’s assistant over the next year. “The Virtual Kidney Check and Follow up in Manitoba will offer an opportunity to reach more people using provincial health information that exists,” explains Martin. “It is an opportunity for the Manitoba Kidney Check team to prioritize in-person screening and an opportunity to continue offering kidney health checks to treat any problems earlier and access resources closer to home.”
Turner says that, despite the challenges that COVID-19 has posed, the BC Kidney Check project will continue to work in collaboration with participating communities and to support their readiness and self-determination to resume screening activities. “A number of communities are participating in virtual training that will allow them to carry out screening activities until we are able to support the screening activities in person,” she says. “This will ensure that more individuals receive timely care and experience better outcomes.”
“A number of communities are participating in virtual training that will allow them to carry out screening activities until we are able to support the screening activities in person. This will ensure that more individuals receive timely care and experience better outcomes.”
Catherine Turner
Senior Research Coordinator, BC Kidney Check
Feature story
Transplant Ambassadors break down barriers to living kidney donation

Transplantation is often the preferred treatment for people with advanced chronic kidney disease. However, patients and donors considering this option do not always receive the information they need to make informed decisions.
To address this gap, a Can-SOLVE CKD research project has launched the Transplant Ambassador Program (TAP), a patient-led initiative that has made great strides in disseminating valuable information about transplantation to both patients and health professionals in renal units across Ontario.
Along with creating educational materials, Transplant Ambassadors make in-person appearances in kidney clinics. Each TAP team member has personal experience with kidney transplantation, either as a donor or recipient. If patients or health professionals in the clinic have questions about transplantation, the TAP patient partners are more than happy to share their real-world experience, answer questions, and dispel myths.
“We want to [break down] the barriers to living donation and we also want to provide information and support to patients along their journey,” explains Marian Reich, a kidney donor who is a Transplant Ambassador in Richmond Hill, Ontario. “People often feel better about transplantation after talking to someone who has done it. They don’t have to feel as afraid, they don’t have to feel as alone. And that’s the rewarding thing – when you can make a difference in someone’s life.”
Based on her experience, Reich has found this approach helpful for addressing misinformation about transplantation. For example, many people think that a donor must be a blood relative, which is not true. As well, some people assume that the recovery time from kidney transplantation is a long process (e.g., six months), when many people have a much quicker recovery time (e.g., six weeks).
Susan McKenzie is a patient partner co-leading the research project and who has been a TAP ambassador since its inception. She received a kidney from Reich, her sister-in-law. McKenzie emphasizes what a difference information from patients, to patients, can make. She says, “This is great, because as patients we know the more we can ‘naturalize the idea of transplantation’ for other patients – by being living breathing, accessible examples of transplant – the less frightening the idea becomes for patients when and if they get to that point in their kidney journey.
“When I was a patient, I never had the benefit of seeing or meeting anyone who had had a successful transplant and the idea was very scary,” says McKenzie.
TAP ambassadors have been making their rounds throughout 13 kidney clinics in Ontario since 2018. Over that same time period, there has been an increase in the number of living donations, although it’s not possible to say with certainty that the TAP program is the underlying reason for this increase. Nevertheless, the TAP ambassadors are pleased. “I’m very thrilled with the progress,” says Reich.
Given how TAP ambassadors typically made in-person visits to kidney clinics, their work was affected by COVID. But when they could no longer do in-person visits, a new opportunity to reach more people emerged through virtual communication. As they shifted to virtual sessions, this allowed ambassadors to reach new patients and health professionals in other locations.
Reich says the TAP team also took the time to gather group profile information on all of the ambassadors (e.g., age, gender, transplantation status). This allows for patients or donor recipients to be better matched with ambassadors with the most relevant experience to that individual.
“So if there is a patient in a centre in Sudbury who wants to connect with an ambassador who has a similar lived background, we could perhaps find one from another active centre,” explains Reich.
There are currently more than 75 TAP ambassadors across Ontario who have completed more than 4,000 face to face meetings between January 2017 and March 2020. TAP is part of the larger Living Donor research project being completed by Can-SOLVE CKD.
Learn more at https://transplantambassadors.ca
“People often feel better about transplantation after talking to someone who has done it. They don’t have to feel as afraid, they don’t have to feel as alone. And that’s the rewarding thing – when you can make a difference in someone’s life.”
Marian Reich
Patient Partner
Connect with us!
Subscribe to learn more about what we do, why it matters, and how you can get involved!